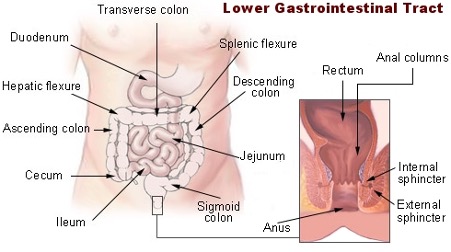
- Lower Gastrointestinal Tract
Consult Dr. Sure Pavan Kumar one of the best gastroenterologists in Vijayawada provides Lower Surgery GI Treatment. MIG Hospital is the top gastroenterology hospital provides Upper GI Tract and Lower GI Tract.
In our body’s intestinal system, the Lower Gastrointestinal Tract (Lower GI Tract) is the segment of gastrointestinal tract including the small intestine below the duodenum, which includes all the components of the ileum, jejunum, the large intestine and the rectum (most distal).
Together, the colon and the rectum make up the bowel, which helps to process and discard of the food we eat. Colorectal diseases refer to conditions impacting the colon or rectum and their functionality, including colon cancer, colon polyps, colitis, and Crohn’s disease. These conditions can range from mild irritations to serious illnesses. Fortunately, a variety of screening and treatment options can help you and your provider pinpoint your specific colorectal condition and help you live the healthiest life possible.
Some major colorectal conditions include:
⦁ Colorectal cancer. Colorectal cancer may develop from colon polyps which have become cancerous.
⦁ Colitis. When the colon becomes inflamed, it is called ulcerative colitis. This condition may occur sporadically or become a chronic illness requiring medications and treatment.
⦁ Crohn’s Disease. Crohn’s disease is an autoimmune disease of the digestive tract that causes inflammation (swelling) in the small intestine or other part of the digestive system.
⦁ Irritable bowel syndrome (IBS). IBS is a common digestive ailment characterized by bloating, cramps, diarrhea, and abdominal pain.
Symptoms
Common signs and symptoms of colorectal conditions include:
⦁ Rectal bleeding. You may see blood in your underwear or on toilet paper after you’ve had a bowel movement.
⦁ Blood in your stool. Blood can make stool look black, or it can show up as red streaks in your stool.
⦁ Abdominal pain. A large polyp can obstruct your bowel and cause cramps and constipation.
⦁ Ongoing constipation or diarrhea. Constipation or diarrhea that last more than a week could also indicate a bowel obstruction.
When to See a Doctor
Causes
Some colorectal conditions may not have a specific cause, while many may be a result of diet and activity. Other causes and risk factors include:
⦁ Age. Most people with colon polyps are over age 50.
⦁ Ethnicity. African Americans have a higher rate of colon polyps than other ethnic groups.
⦁ Family history. Polyps, colon cancer, or other diseases of the colon often run in the family.
⦁ Sedentary lifestyle. Inactivity slows your digestion and waste stays in your colon longer. This may increase colorectal problems.
⦁ Smoking and alcohol. Smoking and drinking alcohol in excess both significantly increase your risk of colon polyps and cancer.
⦁ Obesity. Being 30 pounds or more overweight encourages the growth of extra cells in the colon and rectum.
⦁ Inherited gene mutations. Some rare inherited conditions can cause hundreds of polyps.
Diagnosis and Tests
To know if you have a colorectal condition, your provider may need to look inside your colon. Procedures to look inside your colon include:
Colonoscopy. A long, flexible tube with a tiny video camera at the end is inserted through your rectum. The doctor can see the entire colon, and can remove most polyps to test for cancer.
⦁ Flexible sigmoidoscopy. This is similar to colonoscopy, but only looks at the first part of your colon.
⦁ Virtual colonoscopy. Using computer images and x-rays, the doctor creates a picture of the inside of your colon. The doctor can see the entire colon, but cannot remove abnormal tissue.
⦁ Barium enema. The inside of your colon is coated with a contrast dye that helps abnormalities show up better on an x-ray. The doctor can see the entire colon, but cannot remove abnormal tissue.
Treatments
Treatments for colorectal conditions differ depending on the type and severity of the problem. Common treatment approaches may include:
⦁ Medication to reduce inflammation or help regain normal bowel functionality
⦁ Surgery to remove polyps or cancerous cells
⦁ Changes to diet or lifestyle
Prevention
You can greatly lower your risk of developing polyps and other colorectal conditions if you:
⦁ Eat more calcium and folate. These minerals have been shown to decrease the size and number of polyps. Foods rich in calcium include milk, cheese, and broccoli. Foods rich in folate include chickpeas, kidney beans, and spinach.
⦁ Eat less fat. Especially limit saturated fats from animal sources such as red meat.
⦁ Eat more fruits, vegetables, and whole grains. Fiber moves food through your colon faster and reduces the amount of time your colon is exposed to any harmful substances.
⦁ Exercise every day. Exercise also moves food through your colon faster.
⦁ Don’t drink much alcohol. Drinking more than one drink a day for women and two drinks a day for men increases your risk of colon cancer.
⦁ Stop smoking. If you can’t stop smoking, then at least cut back.
⦁ Lose extra weight. Fat encourages the growth of cells in the colon
Disorders
⦁ Intestinal perforation
⦁ Intestinal obstruction- adhesions from previous surgery, Tuberculosis, Crohns disease, other diseases
⦁ Enterocutaneous fistula
⦁ Small bowel diarrhea\
⦁ Intestinal tumors
⦁ Intestinal gangrene
Colonic and rectal disorders
⦁ Colonic diverticulosis
⦁ Constipation
⦁ Piles (Hemorrhoids), Fissure
⦁ Abscess-peri anal
⦁ Rectovaginal fistula
⦁ Rectal prolapse
⦁ Colonic obstruction- volvulus
⦁ Lower GI bleeding
⦁ Inflammatory bowel disease- Crohns disease, Ulcerative colitis
⦁ Colorectal cancers
Various surgical procedures
⦁ Diagnostic laparoscopy
⦁ Hemicolectomy
⦁ Total colectomy
⦁ Anterior resection
⦁ Low anterior resection
⦁ Ileal pouch surgery
⦁ Rectopexy
⦁ Small bowel resection
⦁ Adhesiolysis
⦁ Bypass surgeries
⦁ Stricturoplasty
⦁ Piles, fistula, perianal abscess surgeries
